Relationship Between Health & Wealth
Residence, itself, is not a risk factor for health insurance status relative to income. Yet in rural America, as elsewhere, health and wealth are intimately linked. Working-age rural adults have higher-than-average rates of unemployment, under-employment, and disability retirement. Moreover, employment opportunities in rural America tend to be at smaller firms, and offer lower wages and fewer benefits. Nearly eighty percent of uninsured rural families have at least one full-time worker.
A number of studies show that degree of rurality is closely correlated with a population’s health, wealth, and overall lifestyle. For example, many rural communities that are adjacent to metropolitan communities not only fare better than remote or isolated rural communities but also the urban centers that they abut. These locales, for example Loudoun County, Virginia or Douglas County, Colorado, are increasingly desirable destinations for residents who want to enjoy the "best of both worlds" – the leisurely pace and recreational opportunities of a pristine natural environment, coupled with the higher wages and access to health care of an urban setting.
Rural Populations and Overall Health
At the population level, rural residents tend to have poorer health than urban residents. They bear a disproportionate burden of chronic diseases including cardiovascular and pulmonary conditions, a number of cancers, diabetes, pre-term/low birth weight, and chronic pain, as well as unintentional injury, motor vehicle accidents, depression, binge drinking, and suicide. Life expectancy among rural populations is lower than their urban counterparts, and in a number of rural locations has fallen in the last ten to twenty years.
| Number of... | Rural U.S | Urban U.S. |
|---|---|---|
| Health Professional Shortage Areas | 2157 | 910 |
| Doctors per 100,000 people | 120 | 300 |
| Primary care doctors per 100,000 people | 52 | 71 |
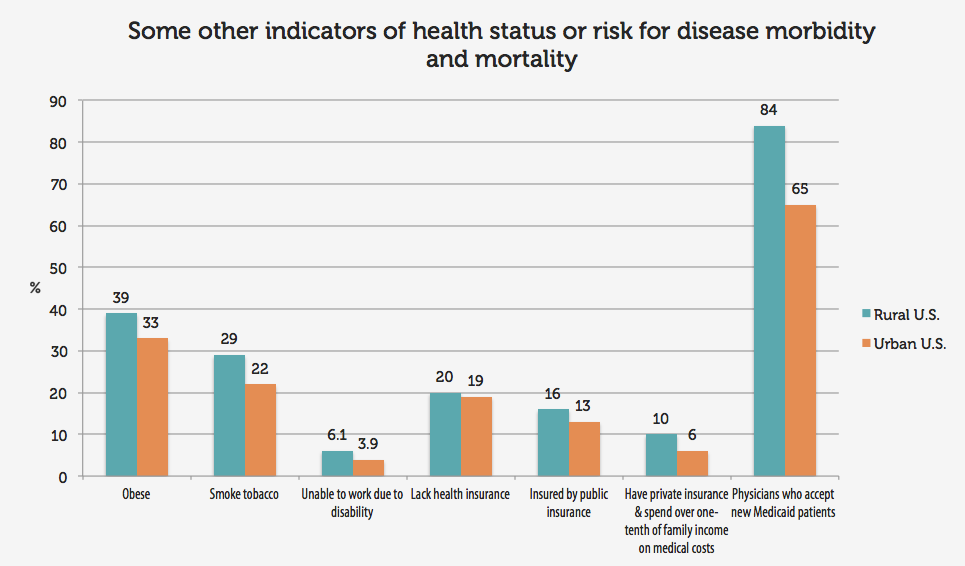
Rural populations also bear a disproportionate burden of risk for disease, from behavioral factors like delayed medical screenings and lack of exercise to structural factors such as insufficient health insurance coverage and inadequate provide-to-patient ratios. For example, 104 rural counties in the United States have no practicing physician, and 136 rural counties have no practicing primary care physician. Eighty-seven percent (87%) of the country’s 1,669 Mental Health Professional Shortage Areas are rural.